想睇中文版?
基本資料
病人資料: 冼某,男/62歲。保險從業員。
過往史:否認藥物、食物敏感。高血壓及高膽固醇史,服藥;鼻敏感史。2021年4月雙目行白內障手術。
現病史:
目赤痕癢四年。
訴於2018年自馬來西亞回港後眼部不適,痕癢、泛紅絲。西醫診為眼部感染,予含類固醇眼藥水,效可。唯病人稱因長期使用含類固醇眼藥水而致雙目病發白內障,已於2021年4月行人工晶體置換手術。然因雙眼痕癢紅絲未去,又不欲再用含類固醇眼藥水,故從妻子建議,前來就診調治。
治療
23.8.2021 初診
刻診訴眼癢,無痛,目[目及]多,質稍干黃,無羞明,不耐風吹,多淚,晨起尤甚。查眼紅絲滿佈。神可。語速略快,聲高。體形適中,膚幽黑。眠可。納佳,無脾胃不適症狀,無噯氣泛酸。無胸脅苦滿,口干多飲,口苦,眼干澀,偶頭痛頭暈,心情易急燥多慮。大便日1行,爛。小便調。平常多汗出。怕熱。偶腰腿酸軟。舌暗紅,瘀點,苔白膩;脈沉弦,數。
診斷:赤目。肝鬱不舒,風熱蘊肺。治以疏肝清肺疏風之法。
治療:處方中藥濃縮藥粉(下同)如下:
銀柴胡,防風,白芍,烏梅,五味子,佛手,桑白皮及柴胡疏肝散。5天,餐後早晚各1服。
方義:以寒熱共濟,收散並舉的過敏煎為主方理肺氣,輔以桑白皮清瀉肺熱,再合柴胡疏肝散及佛手理肝氣,以圖疏肝解鬱,散風清熱之效。
6.9.2021 二診 (因期間打疫苗針,故在針後停服中藥,代盡劑後再來復診)
報藥後病情改善,查紅絲亦較前診減少,但仍不時見癢。患者亦已刻意減少含類固醇眼藥水,並改用人工淚液。另訴近周眠差寐淺,醒後難復眠,報因生意不佳而起憂慮故,亦憂心將考DSE兒子的情緒及學業。餘證同前。舌暗紅,瘀點,苔黃(染)膩;脈沉弦,略數。為對應兩個不同的病,擬兩方分服如下:
方一:
銀柴胡,防風,白芍,烏梅,五味子,佛手,桑白皮,柴胡疏肝散及 龍膽瀉肝湯。6天,早上餐後1服。
方義:同上。因取效,故在前方上疏肝之上,酌加3克更能瀉肝之龍膽瀉肝湯以以清瀉肝鬱之火。而藥量又從12克加至15克一服。
方二:
桂枝,生薑,牡蠣,黃芩,黨參,大棗,柴胡,大黃,龍骨,煅磁石,茯神,酸棗仁(炒)及 合歡皮。6天,晚上餐後1服。
方義:心有所思,則神魂浮動;神魂浮動,則夜寐不安,故以柴胡加龍骨牡蠣湯加酸棗仁及合歡皮取和解清熱,鎮驚安神之效。
15.9.2021 三診
報藥後眼疾已去八九 ── 痕癢大減,紅絲去。能不再用含類固醇眼藥水,已可用人工淚水代之。眠在藥後亦有改善,停藥後未有復發。唯報服藥後大便未能如前一次排清,而要分作兩次而清,成形。另訴有腸鳴、噯氣及矢氣,亦欲調之。因眠已改善,故去助眠之方,轉服補脾益氣及行氣之劑。舌暗紅,苔薄白;脈濡,略弦。因發新證,亦擬兩方分服如下:
方一:
銀柴胡,防風,白芍,烏梅,五味子,佛手,桑白皮,柴胡疏肝散及龍膽瀉肝湯。6天,早上餐後1服。
方義:同上。守方,以鞏固療效。
方二:
厚朴,枳實(麩炒),佛手,五爪龍及 參苓白朮散。6天,晚上餐後1服。
方義:其中焦證,皆是氣虛氣滯之象,故以參苓白朮散合性平益氣的五爪龍補脾益氣,並輔以厚朴、枳實及佛手解其氣滯。
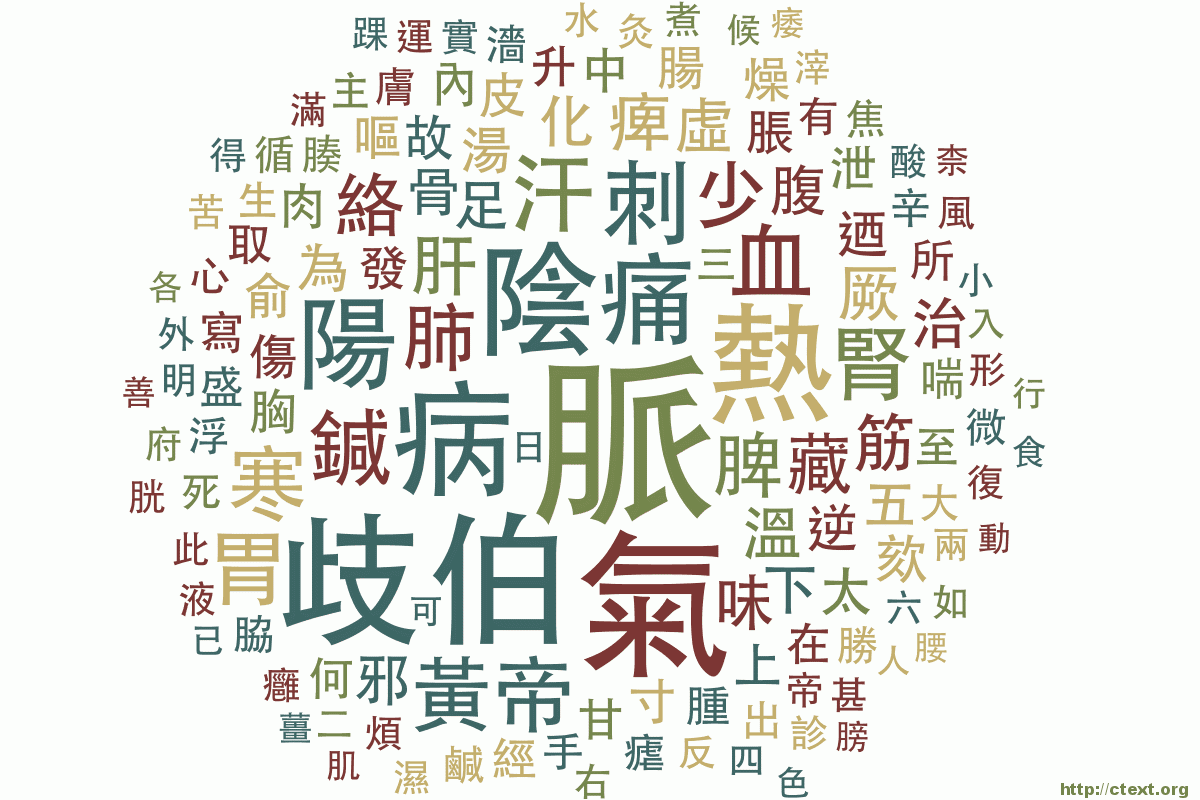
病理概要
目赤,俗稱「火眼」、「紅眼」。是指雙眼(或單眼)白睛見紅赤。患者主訴正合此義。目赤證型繁多,如有外感風熱、肝膽火盛、邪熱伏絡及酒毒內蘊等實證,亦可見如肝腎陰虛等因虛火而有的證型;更有具傳染性的天行赤眼。《銀海指南.卷一.火》給出一個很精闢的總結 ── 「目不因火則不病,白輪變赤,火乘肺也」,其扼要地指出了病邪為火,病位總關及肺。目赤的辨證,首辨虛實,實者發病急,虛者發病慢。實者又當再辨外感、內傷。
另外,外感目赤,傳染以致流行者,為天行時邪目赤。傳染性較差,不致流行者,為一般外感風熱。因肝火而目赤者兼有裡熱證,外感則兼表熱證。虛者以肝腎陰虧為多。但亦有虛實夾雜者,又當酌情治以攻補兼施之法。
思路及體會
依五輪及臟象辨證:由於白睛屬肺,目為肝竅,又不見他臟或經絡作病之顯證,所以當從肝肺二臟入手。病起之初,發於由熱帶地區(馬來西亞)回港後,當可疑外感風熱為其病本,惜因失治而病程遷延4年。加之患者素有鼻敏感史,亦疑其為敏感體質,因此基於發病的時間及有鼻敏感史這兩個提示,方選祝諶予老先生的過敏煎合桑白皮理肺之風熱二邪。肝鬱之證,則治以柴胡疏肝散合佛手以理肝氣。本想當用龍膽瀉肝湯,但因是初診,未能掌握患者體質,故亦想以柴胡疏肝散作投石問路之用。在二診得知對證後,亦即酌加3克的龍膽瀉肝湯,以清瀉肝火。現在看來,在二及三診時實已可去柴胡疏肝散,使藥力更專。
另外,二三診之不寐及大便習慣改變,可因於環境及情志的影響,亦不排除是用藥的結果。但體會到在用藥上,總得要守住主證,不要被症狀牽著鼻子走。在治療主證外,或許那句「有是證,用是方」可資參考。為了同時兼顧兩個病,早晚分服不同藥方,亦可為權宜之計。
Basic Information
Patient Information
Mr. Xian, Male/62 years old. Insurance employee.
Medical History
Denies medication and food allergies. History of hypertension and high cholesterol, currently medicated; history of nasal allergies. Bilateral cataract surgery performed in April 2021.
Present Illness
Itchy red eyes for four years.
Complains of discomfort in the eyes since returning from Malaysia in 2018, with itching, redness, and irritation. Diagnosed with eye infection by Western medicine and prescribed steroid eye drops, which provided relief. However, prolonged use of steroid eye drops led to bilateral cataracts, with surgery performed in April 2021. Despite the surgery, persistent itching and redness remained, and the patient preferred not to use steroid eye drops again. Following his wife’s advice, he sought traditional Chinese medicine treatment.
Treatment
August 23, 2021 – Initial Consultation
Complains of itchy eyes, non-painful, tearing, slightly dry with yellow discharge, sensitive to wind, excessive tearing, worse in the morning. Examination shows redness in the eyes. Mentally alert, speech slightly rapid and loud. Moderate build, dark complexion. Normal sleep, good appetite, no gastrointestinal symptoms, no chest discomfort, occasional headache and dizziness, easily irritable and anxious. Bowel movements once a day, loose. Normal urination. Sweats easily, heat intolerance, occasional lower back and leg soreness. Tongue dark red with ecchymosis, white greasy coating; pulse deep and string-like, slightly rapid.
Diagnosis: Conjunctivitis. Liver depression with lung heat and wind-heat syndrome. Treatment with methods to soothe the liver, clear the lungs, and dispel wind.
Treatment: Prescribe concentrated herbal powder as follows:
Yin Chaihu, Fang Feng, Bai Shao, Wumei, Wuweizi, Foshou, Sangbaipi, and Chaihu Shugan San. 5 days, one dose after breakfast and dinner.
Rationale: Cold and heat balance, dispersing and soothing allergy decoction as the main treatment principle to regulate lung qi, supplemented by Sangbaipi to clear lung heat, combined with Chaihu Shugan San and Foshou to regulate liver qi, aiming to soothe liver stagnation, dispel wind, and clear heat.
September 6, 2021 – Second Consultation (Treatment interrupted due to vaccination, resumed after completing the dose)
Symptoms improved after taking medicine, decreased redness in the eyes, but occasional itching persists. Patient deliberately reduced the use of steroid eye drops and switched to artificial tears. Also reports recent sleep disturbances and worries about business and his son’s DSE exam. Other symptoms unchanged. Tongue dark red with ecchymosis, yellowish (stained) coating; pulse deep and string-like, slightly rapid. Considering two different conditions, two separate treatments are proposed:
Prescription One:
Yin Chaihu, Fang Feng, Bai Shao, Wumei, Wuweizi, Foshou, Sangbaipi, Chaihu Shugan San, and Longdan Xiegan Tang. 6 days, one dose after breakfast.
Rationale: Similar to previous treatment with an addition of Longdan Xiegan Tang to further clear liver fire. The dosage is increased from 12g to 15g per dose due to improved efficacy.
Prescription Two:
Guizhi, Shengjiang, Muli, Huangqin, Dangshen, Dazao, Chaihu, Dahuang, Longgu, Duan Cishi, Fushen, Suanzaoren (fried), and Hehuanpi. 6 days, one dose after dinner.
Rationale: Considering the patient’s restless sleep, Chaihu plus Longgu and Muli Decoction with Suanzaoren and Hehuanpi are prescribed to harmonize and calm the spirit.
September 15, 2021 – Third Consultation
After medication, eye symptoms significantly improved, itching greatly reduced, redness disappeared. No longer needs steroid eye drops and can use artificial tears instead. Sleep has also improved after medication, with no relapse after discontinuing medication. However, bowel movements are not as smooth as before, requiring two separate sessions for complete evacuation. Also complains of abdominal rumbling, belching, and flatulence, seeking relief. Tongue dark red, thin white coating; pulse moist, slightly string-like. Due to the new symptoms, two separate treatments are proposed:
Prescription One:
Same as before. 6 days, one dose after breakfast.
Rationale: Same as before, to consolidate the treatment effect.
Prescription Two:
Houpo, Zhishi (fried), Foshou, Wuzhualong, and Shenlingbaizhusan. 6 days, one dose after dinner.
Rationale: Symptoms of abdominal discomfort are indicative of spleen deficiency and qi stagnation. Shenlingbaizhusan combined with the mildly warming Wuzhualong and Foshou is prescribed to strengthen the spleen and invigorate qi, supplemented with Houpo and Zhishi to resolve qi stagnation.
Summary of Pathology
Conjunctivitis, commonly known as “red eye” or “pink eye,” refers to redness in the white part of one or both eyes. The patient’s complaints align with this condition. Conjunctivitis can manifest in various patterns, including external wind-heat, liver-gallbladder fire, hidden heat in the lungs, and internal accumulation of heat from alcohol. Additionally, there is the infectious epidemic form known as epidemic conjunctivitis. Diagnosis involves differentiating between excess and deficiency, with excess patterns manifesting acutely and deficiency patterns developing slowly. Excess patterns may further be differentiated into external wind-heat and internal injury.
Reflections
Based on the theory of the Five Wheels and organ patterns: Since the white part of the eyes is associated with the lungs and the eyes are the “window of the liver,” and there are no clear signs of other organ or meridian involvement, treatment should focus on the liver and lungs. Initially, the patient’s condition likely stemmed from external wind-heat after returning from a tropical climate (Malaysia), but unfortunately, it was not promptly treated, resulting in a four-year course of illness. Considering the patient’s history of nasal allergies, an allergic constitution is suspected. Therefore, based on the onset time and the history of nasal allergies, the prescription of Zhu She Yu’s allergy decoction combined with Sangbaipi to regulate lung qi and treat wind-heat was chosen. For liver depression syndrome, Chaihu Shugan San combined with Foshou to regulate liver qi was prescribed. Originally, Longdan Xiegan Tang was considered, but due to the initial consultation, the patient’s constitution was not fully understood, so Chaihu Shugan San was used as an exploratory treatment. After understanding the condition in the second consultation, Longdan Xiegan Tang was added to further clear liver fire. Now, it appears that Chaihu Shugan San can be discontinued at the second and third consultations to enhance the efficacy of the treatment.
Additionally, the insomnia and changes in bowel habits during the second and third consultations may be influenced by environmental and emotional factors, possibly as a result of medication. However, it is essential to maintain focus on the primary condition in treatment and not be led solely.